Men in the UK die nearly four years earlier than women on average, with shocking disparities in preventable deaths from heart disease, accidents, and suicide. As England prepares its first men’s health strategy, experts reveal why men struggle to care for their wellbeing – and what can change this dangerous trend.
Why Men’s Health Lags Behind
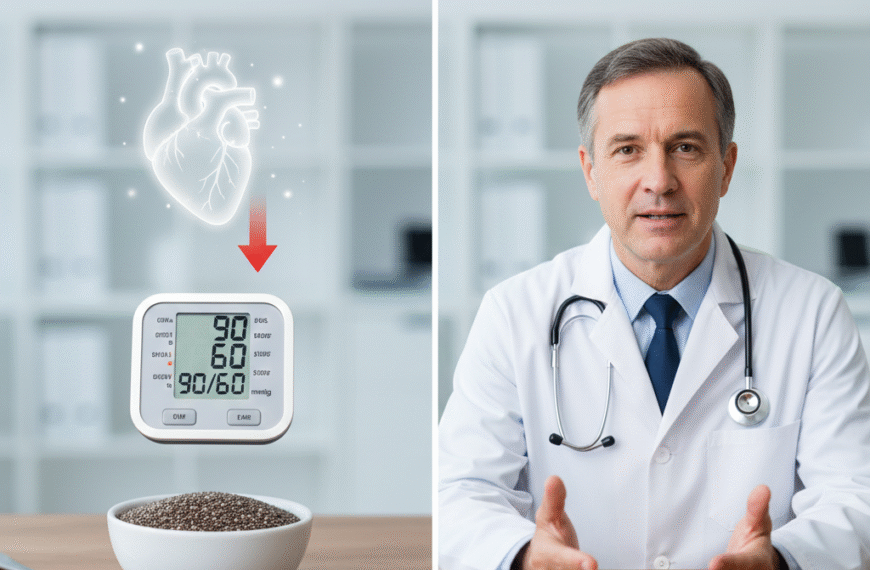
The statistics paint a grim picture: men are 60% more likely to die before age 75 than women. They’re also less likely to visit doctors, attend health screenings, or seek help for mental health issues. According to Professor Alan White of Leeds Beckett University, this isn’t just about lifestyle choices – it’s a perfect storm of biological, social and systemic factors.
“Men have weaker immune responses, poorer health literacy, and often lack the skills to navigate healthcare systems,” explains White. While women regularly interact with health services through contraception, cervical screenings and childbirth, many men go decades without seeing a medical professional.
Cultural expectations compound the problem. “Society tells men to ‘man up’ and endure pain silently,” says Mark Brooks of the All-Party Parliamentary Group on Men’s Health. This toxic masculinity leads men to ignore warning signs until it’s too late – like construction workers hiding chronic pain for fear of losing their jobs.

The Inequality Factor
Deprivation dramatically worsens these trends. In England’s poorest areas, men die 10 years younger than in wealthy neighborhoods – a larger gap than seen among women. Blue-collar workers face particular challenges, with just 40% attending NHS health checks due to work pressures and difficulty accessing services.
Ethnic disparities add another layer: Black men face double the prostate cancer risk, while South Asian men are disproportionately affected by diabetes. “Our one-size-fits-all healthcare system fails to address these differences,” Brooks notes.
Turning the Tide
Innovative programs show promise in bridging this gap:
- The Movember Foundation’s “mental fitness” program teaches men to track moods through action-oriented goals like sports or social activities
- Men’s Sheds create safe spaces for camaraderie while working on practical projects
- Workplace initiatives could provide paid time for health checks at industrial sites
Professor Paul Galdas of York University emphasizes: “Men engage best with health when it’s activity-based, not just talking in clinics.” His research shows men will open up when approached through sports, hobbies or workplace programs.
What Needs to Change

Experts call for:
✅ A national men’s health strategy mirroring England’s women’s health initiative
✅ Workplace health rights including paid time for medical appointments
✅ Community-based services in gyms, pubs and workplaces
✅ Better mental health support recognizing male-specific symptoms like anger or substance use